Causes and Risk Factors for PAD
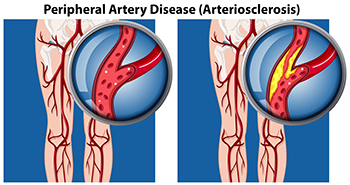
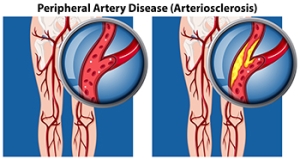
Peripheral artery disease, or PAD, occurs when plaque builds up in the arteries, causing reduced blood flow to the lower limbs. This leads to such symptoms as pain, cramping, or numbness in the feet, toes, or ankles. Smoking, diabetes, high blood pressure, and high cholesterol are major risk factors, while aging and a family history of vascular disease can also contribute to its development. Poor circulation from PAD may cause slow-healing wounds, skin discoloration, and, in severe cases, ulcers that increase the risk of infection or limb loss. A podiatrist can evaluate the blood flow to the feet and ankles, identify complications, and recommend appropriate treatment to help prevent more serious outcomes. Depending on the severity of the peripheral artery disease, treatment may include medical management or procedures like angioplasty or bypass surgery. If you are experiencing foot problems related to peripheral artery disease, it is suggested that you visit a podiatrist for guidance and treatment options.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Desiree Garzon, DPM from County Wide Foot, Ankle, & Wound Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Boynton Beach, and Wellington, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Reasons to Visit a Podiatrist

Many people experience foot, toe, or ankle problems, either due to chronic health conditions like diabetes and arthritis, or from everyday factors such as wearing ill-fitting shoes or participating in strenuous activities like running. Podiatrists specialize in diagnosing and treating a wide range of foot, toe, and ankle conditions, providing relief through medication, specialized footwear recommendations, or surgery, when needed. Athletes frequently encounter injuries like sprains or shin splints, and a podiatrist can identify underlying issues and suggest preventive measures. Painful conditions like heel spurs, bunions, or ingrown toenails require professional intervention, as podiatrists can effectively manage these issues through targeted treatments or surgical correction. Diabetic patients benefit significantly from regular podiatric care, as it reduces the risk of severe complications, including infections that could lead to loss of limb. Conditions like persistent athlete’s foot, corns, or calluses also require expert care to achieve lasting relief. When you have foot, toe, or ankle problems, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Desiree Garzon, DPM from County Wide Foot, Ankle, & Wound Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our offices located in Boynton Beach, and Wellington, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
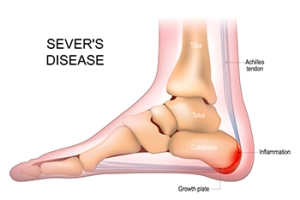
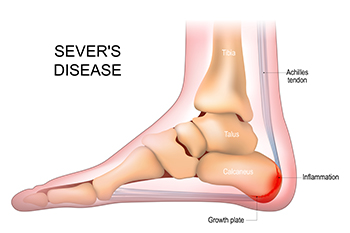
Managing Sever’s Disease
Sever's disease, also known as calcaneal apophysitis, is a foot condition in growing children, particularly those active in sports. It occurs when the growth plate in the heel becomes irritated, causing pain and swelling in the heel. Symptoms typically include pain at the back or bottom of the heel, especially after physical activity or prolonged standing. The pain may be sharp or aching, and the child may have difficulty walking or running without discomfort. A podiatrist can help diagnose Sever’s disease through a physical exam and may suggest treatments to alleviate pain and reduce inflammation. This type of doctor can provide guidance on stretching exercises, custom orthotics, or cushioned heel pads to help relieve pressure on the heel. In some cases, changes in footwear or activity level may be necessary to prevent further irritation. If your child has heel pain, it is suggested that you schedule an appointment with a podiatrist who can effectively manage Sever's disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see Desiree Garzon, DPM from County Wide Foot, Ankle, & Wound Care. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Boynton Beach, and Wellington, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
Taking Care of Your Diabetic Feet

Diabetic foot care is essential for anyone with diabetes, as high blood sugar can lead to nerve damage, called neuropathy, and poor circulation. These issues make it harder to feel injuries or detect infections, which can lead to serious complications, if untreated. Symptoms include numbness, tingling, or a burning sensation in the feet. You might also notice cuts, blisters, or ulcers that heal slowly, along with swelling or redness. If left untreated, infections can worsen, leading to more severe conditions, including limb loss. To prevent complications, daily foot inspections are critical. It is important to look for cuts, sores, or swelling. Keep your feet clean and dry, wear properly fitted shoes, and avoid tight socks. Controlling your blood sugar and avoiding smoking can improve circulation. A podiatrist can help with regular foot exams and early detection of wounds or ulcers. This foot doctor also can provide treatment for existing issues like wound care or prescribe custom orthotics for better foot alignment. For comprehensive diabetic foot care, it is suggested that you schedule an appointment with a podiatrist.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Desiree Garzon, DPM from County Wide Foot, Ankle, & Wound Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Boynton Beach, and Wellington, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Men and Women’s Running Shoes

When selecting running shoes, both men and women should consider their specific needs, such as the type of running they do and their foot structure. For those who run on roads or hard surfaces, cushioned running shoes are ideal as they provide ample shock absorption. Trail runners, on the other hand, benefit from shoes with more grip and durability, designed to handle uneven terrain. Stability shoes are great for individuals with mild overpronation, offering support to keep the foot aligned while running. Neutral shoes are suited for runners with a natural gait, offering flexibility and comfort. For both men and women, finding the right fit is essential, as wearing improper shoes can lead to discomfort or injury. Factors like arch height, foot shape, and running style should guide the decision. If you have endured a foot injury from running, it is suggested that you consult a podiatrist who can offer effective relief and treatment tips, and guide you the right type of running shoes to wear.
If you are a runner, wearing the right running shoe is essential. For more information, contact Desiree Garzon, DPM from County Wide Foot, Ankle, & Wound Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Choosing the Right Running Shoe for Your Foot Type
To increase performance and avoid the risk of injury, it is important to choose the right running shoe based on your foot type. The general design of running shoes revolves around pronation, which is how the ankle rolls from outside to inside when the foot strikes the ground.
- Neutral runners are able to choose from a wide variety of shoes, including minimalist shoes or even going barefoot.
- Runners who overpronate, or experience an over-abundance of ankle rolling, should choose shoes that provide extra motion control and stability.
- Runners who underpronate, or supinate, have feet that have high arches and lack flexibility, preventing shock absorption. They require shoes with more flexibility and cushion.
If you have any questions please feel free to contact our offices located in Boynton Beach, and Wellington, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.